What is Addison’s Disease?
Addison’s disease is a rare and potentially life-threatening disorder characterized by the insufficient production of hormones from the adrenal glands, specifically cortisol and aldosterone. These glands, located on top of each kidney, play a critical role in regulating various physiological processes, including metabolism, immune response, and blood pressure. The deficiency of these hormones can lead to a cascade of health issues that affect multiple organ systems.
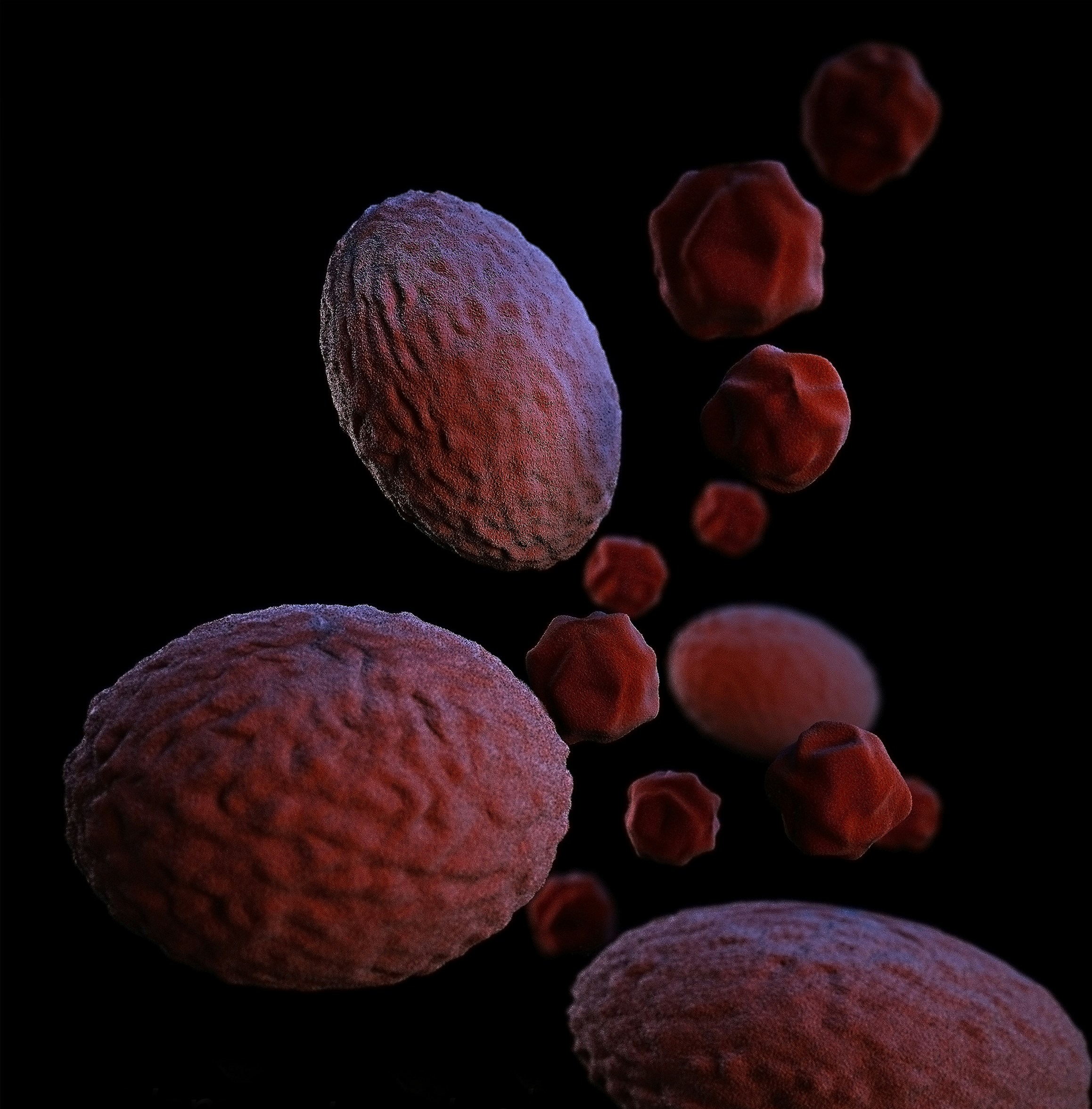
The primary cause of Addison’s disease is often attributed to autoimmune destruction of the adrenal cortex, the outer layer of the adrenal glands. In this scenario, the body’s immune system mistakenly attacks its own adrenal tissue, resulting in hormonal deficiencies. Additionally, other factors may contribute to adrenal insufficiency. These include infections such as tuberculosis and fungal diseases, which can damage the adrenal glands, as well as genetic predispositions that can lead to adrenal dysfunction.
More informationUnderstanding the Latest Stroke Prevention Guidelines: What You Need to KnowMoreover, certain medications, like those that affect cortisol synthesis, and conditions such as bilateral adrenalectomy, where both adrenal glands are surgically removed, can also precipitate Addison’s disease. In some cases, adrenal insufficiency may arise as a component of a syndrome, such as polyglandular autoimmune syndrome, where multiple endocrine glands are affected. It is essential for individuals experiencing symptoms such as fatigue, weight loss, low blood pressure, and skin changes to seek prompt medical consultation.
Understanding the intricacies of Addison’s disease is vital for accurate diagnosis and effective treatment. Early detection is key, as untreated adrenal insufficiency can lead to an adrenal crisis, a serious and potentially fatal condition. By recognizing the causes and symptoms associated with this disorder, patients and healthcare providers can work together toward an effective management plan.
Key Symptoms of Addison’s Disease
Addison’s disease, a disorder of the adrenal glands, manifests through a variety of symptoms that can significantly affect an individual’s quality of life. One of the most common symptoms is profound fatigue, which often leads to decreased energy levels and an overwhelming sense of tiredness that is not alleviated by rest. This fatigue can hinder daily activities and impact overall wellness.
More informationBird Flu Outbreak: Investigating Human Infections and ResponsesIn addition to fatigue, muscle weakness is a prevalent symptom, which may vary in severity for different individuals. Patients often experience a notable decline in muscular strength, making physical tasks seem more difficult. This weakness can be particularly alarming as it may interfere with routine activities, exacerbating feelings of helplessness.
Weight loss is another symptom that often accompanies Addison’s disease. Individuals may notice a significant drop in weight due to decreased appetite and alterations in metabolism. This unintentional weight loss is often combined with gastrointestinal symptoms such as nausea, which can further contribute to an overall feeling of ill health.
Low blood pressure is also a critical sign of Addison’s disease. Patients may experience orthostatic hypotension, a condition where blood pressure drops significantly upon standing, leading to dizziness or lightheadedness. This fluctuation in blood pressure can pose risks during everyday activities, especially if the individual is not aware of their condition.
More informationThe Surging Cases of Walking Pneumonia Among Young Children: What You Need to KnowSkin darkening, known as hyperpigmentation, is another notable symptom. It often presents as a tan or bronze hue, particularly in areas exposed to sunlight. This discoloration occurs due to increased levels of the hormone adrenocorticotropic hormone (ACTH), which reacts with skin cells. Recognizing these symptoms early is paramount for timely diagnosis and intervention, ultimately facilitating effective treatment and management of Addison’s disease.
The Role of Hormones in Addison’s Disease
Addison’s disease is primarily characterized by a deficiency in hormones produced by the adrenal glands, notably cortisol and aldosterone. Cortisol, often termed the “stress hormone,” plays a critical role in regulating various bodily functions, including metabolism, immune response, and blood pressure. In the absence of adequate cortisol levels, individuals may experience fatigue, weight loss, and mood disturbances, as the body struggles to maintain homeostasis under stress.
Aldosterone, on the other hand, is essential for sodium and potassium balance in the body. It aids in the regulation of blood pressure by promoting the retention of sodium and the excretion of potassium in the kidneys. When aldosterone levels are insufficient, patients may face hypotension, leading to symptoms such as dizziness and even fainting upon standing—a condition known as orthostatic hypotension. Furthermore, inadequate aldosterone affects the kidneys’ ability to manage electrolytes, often resulting in an imbalance that can exacerbate overall health issues.
More informationNewer Mpox Strain: A Growing Concern for Young Women and GirlsThe interplay between cortisol and aldosterone is vital for sustaining bodily functions that encompass stress response and metabolic processes. The deficiency of these hormones in Addison’s disease disrupts the body’s equilibrium, leading to the symptoms that are commonly associated with the condition. Individuals with Addison’s disease may also face challenges in coping with physical stressors, such as illness or injury, due to the lack of cortisol’s protective effects. Moreover, both hormones play a role in maintaining energy levels and overall vitality, showcasing their importance in everyday life.
This intricate hormonal relationship exemplifies why timely diagnosis and management of Addison’s disease are crucial. Understanding the roles of cortisol and aldosterone not only underscores their physiological significance but also aids in appreciating the broader impacts of hormonal imbalance on health.
Diagnosis of Addison’s Disease
Diagnosing Addison’s Disease involves a comprehensive approach that includes evaluating medical history, conducting physical examinations, and performing specific diagnostic tests. A thorough medical history is crucial as it helps healthcare providers understand any previous symptoms, such as fatigue, weight loss, and skin changes, which may indicate adrenal insufficiency. During the physical examination, doctors often look for signs that suggest hormonal imbalances, such as low blood pressure, hyperpigmentation of the skin, and electrolyte imbalances.
More informationUnderstanding Delta Airlines Retirement Age and BenefitsOne of the primary tests used in diagnosing Addison’s Disease is the adrenocorticotropic hormone (ACTH) stimulation test. This test assesses how well the adrenal glands respond to ACTH, a pituitary hormone that stimulates cortisol production. In a healthy individual, the adrenal glands will produce increased levels of cortisol when exposed to ACTH. However, if the adrenal glands are not functioning properly, as in the case of Addison’s Disease, cortisol levels will remain low. This response is indicative of primary adrenal insufficiency.
In addition to the ACTH stimulation test, blood tests are essential in diagnosing Addison’s Disease. These tests check for low levels of cortisol and aldosterone, as well as elevated levels of ACTH. They can also help to identify any associated electrolyte imbalances, such as low sodium and high potassium levels, which frequently occur in patients with the disease. Another useful test can involve 24-hour urine collection to measure cortisol levels, providing further evidence of adrenal function.
Accurate diagnosis is vital as it directly impacts the management and treatment options available for those affected by Addison’s Disease. Misdiagnosis can lead to inadequate treatment and worsening symptoms, making it critical for healthcare providers to utilize a combination of techniques to reach a conclusive diagnosis while considering the challenges that may arise during this complex process.
More informationImpact of Florida Blue and Baptist Health Negotiations on Patients and ProvidersUnderstanding Addisonian Crisis
Addisonian crisis is a severe and potentially life-threatening condition that occurs due to insufficient levels of cortisol in the body, usually as a result of untreated Addison’s Disease. This crisis can arise suddenly, often triggered by factors such as infections, physical stress from surgery or injury, or abrupt withdrawal from steroid medications. Additionally, individuals with undiagnosed Addison’s disease may experience their first symptom through an Addisonian crisis, making it essential for patients and caregivers to be vigilant about the signs and symptoms associated with this acute condition.
The symptoms of an Addisonian crisis can be quite severe and include extreme fatigue, abdominal pain, nausea, vomiting, and confusion. Patients may also experience a significant drop in blood pressure, leading to dizziness or fainting. In many cases, patients may appear very weak, and their skin may exhibit a darker pigmentation, a hallmark of adrenal insufficiency. Rapid medical intervention is critical, as failure to address these symptoms can lead to shock, organ failure, and ultimately, death.
Understanding the triggers and signs of an Addisonian crisis is vital for effective management and prevention. It is important for those diagnosed with Addison’s Disease to carry a medical alert identification at all times. Their caregivers should also be educated on recognizing the symptoms and the immediate actions to take, which may include administering an injection of hydrocortisone, if prescribed, while waiting for emergency medical services. Early recognition and treatment can significantly improve outcomes and save lives.
More informationThe Right to Bear Arms: Understanding Self-Defense and Personal ProtectionTreatment Options for Addison’s Disease
Treatment for Addison’s disease primarily revolves around hormone replacement therapy, which is essential for managing the deficiency of adrenal hormones. The most common approach involves administering synthetic cortisol, known as hydrocortisone, which helps to mimic the body’s natural hormone levels and enables patients to function normally. In some cases, fludrocortisone may also be prescribed to assist with electrolyte balance, specifically sodium retention and potassium regulation. By adhering to the prescribed medication regimen, individuals can effectively manage their symptoms and maintain their health.
Additionally, lifestyle modifications play a critical role in the comprehensive management of Addison’s disease. It is vital for patients to adopt a well-balanced diet that is rich in nutrients and supports adrenal health. Consuming an adequate amount of salt may be beneficial, as individuals often experience low sodium levels due to their condition. Regular physical activity is recommended, but it is important for patients to listen to their bodies and adjust their exercise intensity based on their energy levels. Furthermore, stress management techniques such as yoga, meditation, and deep breathing exercises can prove helpful, as stress can exacerbate symptoms.
Follow-up care with healthcare providers is equally important in ensuring optimal management of Addison’s disease. Routine monitoring of hormone levels, electrolytes, and overall health helps healthcare professionals adjust treatment plans as necessary. Patients should remain vigilant about reporting any changes in symptoms or new health issues, as this information can facilitate timely interventions. By collaborating closely with their healthcare team and committing to both medication and lifestyle changes, individuals can effectively manage Addison’s disease, leading to an improved quality of life.
More informationCoping with Election-Related Stress: Expert Tips and StrategiesLiving with Addison’s Disease
Individuals living with Addison’s disease face unique challenges that significantly impact their day-to-day lives. This condition, characterized by insufficient production of adrenal hormones, necessitates effective management strategies to maintain health and well-being. A cornerstone of coping with Addison’s disease is consistent medication adherence, typically involving the lifelong use of hormone replacement therapy. Patients are often advised to carry emergency injectable medications, especially in situations that may induce an adrenal crisis.
In managing their condition, establishing a strong support system is vital. Friends, family, and caregivers play an integral role in helping individuals navigate the complexities associated with Addison’s disease. Support groups, whether in-person or online, provide a platform for sharing experiences and receiving emotional support. Connecting with others who understand the challenges of living with this condition can create a sense of community, helping to alleviate feelings of isolation.
Stress management is another crucial aspect for those with Addison’s disease. Stress can exacerbate symptoms, making it essential to develop coping techniques that promote relaxation and emotional stability. Techniques such as mindfulness meditation, yoga, and deep-breathing exercises are beneficial in managing daily stressors. Regular physical activity, tailored to individual capabilities, can also enhance overall well-being and resilience.
More informationMichigan Election Day Weather Forecast: What to ExpectAside from physical measures, monitoring one’s mental health is equally important. Psychological support through counseling or therapy can assist individuals in coping with the emotional ramifications of living with a chronic condition. Overall, living with Addison’s disease requires a proactive and holistic approach, recognizing the interplay between physical health, emotional well-being, and supportive relationships. With proper care and a solid support framework, individuals can lead fulfilling lives despite the challenges posed by Addison’s disease.
Research and Future Directions
Addison’s Disease, characterized by the inadequate production of adrenal hormones, has garnered significant attention within the medical research community. Recent advancements in medical science seek to deepen the understanding of this condition and develop more effective treatments. Researchers are focusing on various aspects of Addison’s Disease, including its etiology, mechanisms, and potential therapeutic targets. A thorough understanding of the underlying pathology is crucial to identifying new pathways for intervention and improving patient outcomes.
One promising avenue of research involves the genetic factors associated with Addison’s Disease. Studies have identified specific genetic markers that may indicate a predisposition to the condition. By leveraging genetic research, scientists hope to develop more personalized treatment plans based on individual genetic profiles. This progress could lead to more effective management strategies and, potentially, the development of novel therapies aimed at restoring adrenal function.
More informationTropical Storm Rafael Forms in the Caribbean: What You Need to KnowAdditionally, emerging therapies such as gene therapy may hold potential for patients suffering from Addison’s Disease. Although still in experimental stages, such approaches aim to correct the hormonal deficiencies at a cellular level. Moreover, investigators are exploring the use of stem cell therapy as a means to regenerate adrenal tissue. These innovative treatments could transform the management of Addison’s Disease in the coming years, providing patients with more options and enhancing their quality of life.
Another critical focus of ongoing research is the psychosocial aspects of living with Addison’s Disease. Strategies to improve mental health, coping mechanisms, and patient support networks are gaining traction, as addressing the comprehensive needs of patients may significantly improve overall well-being. As our understanding of Addison’s Disease continues to evolve, the importance of ongoing research cannot be overstated. A collaborative effort among researchers, clinicians, and patients will be essential to advance knowledge, refine treatment strategies, and ultimately improve patient care.
Frequently Asked Questions about Addison’s Disease
Addison’s disease, a disorder of the adrenal glands, often raises numerous questions among those affected and their families. One common inquiry is regarding risk factors for the disease. Addison’s disease can affect individuals of any age, gender, or ethnicity; however, it is more prevalent in adults aged 30 to 50. Autoimmune conditions and certain genetic predispositions may increase one’s risk. Individuals with other autoimmune disorders, like Type 1 diabetes and thyroid disease, are also at a higher risk for developing Addison’s disease.
More informationNew Study Reveals Impact of Ozempic and Wegovy on Knee Osteoarthritis Pain in Obesity PatientsAnother frequent concern pertains to lifestyle choices, particularly diet and exercise. While no specific diet can cure Addison’s disease, maintaining a balanced diet rich in essential nutrients is crucial for supporting overall health. Patients are often advised to consume adequate salt, especially during periods of illness or hot weather, as the body may require increased sodium to compensate for the hormone deficiency. Regular, moderate exercise is encouraged, as it helps improve overall well-being and may mitigate feelings of fatigue commonly associated with Addison’s disease. However, individuals should listen to their bodies and adjust their physical activity levels according to their energy and strength.
Emergency situations also need careful consideration. Those diagnosed with Addison’s disease should always carry an emergency identification card or wear a medical alert bracelet, indicating their condition. Sudden stress, infections, or injuries can trigger an adrenal crisis, a life-threatening situation. It is crucial for individuals to recognize the warning signs of an adrenal crisis, which include severe weakness, confusion, and low blood pressure. Family members and friends should be educated on how to respond in such emergencies, including administering injectable hydrocortisone if available.
By addressing these common questions, we aim to clear up misconceptions about Addison’s disease and encourage those affected to take proactive measures in managing their health.
More informationNavigating the Future of Staking Authority: Tradeoffs and Next Steps More informationEverything You Need to Know to Vote in Ohio: A Guide to VoteOhio.gov- Trump Cabinet Background Checks, Inflation Outlook, More
- Trump Cabinet Picks Reactions, Markets Week Ahead, More
- Trump Chooses Bessent for Treasury in a Nod to Wall Street
- Trump’s Treasury Pick May Spur Relief Rally
- How Saudi Aramco’s CFO Thinks About Dividends
- US retailers stretch out Black Friday deals to lure flagging shoppers
- ‘Wicked’ and ‘Gladiator II’ give Hollywood hope for strong holiday box office
- Sweating the small stuff could work for Argentina
- Palace intrigue over Trump’s nominations grips winter White House
- Assisted dying bill splits UK cabinet ahead of vote
- New Universal Theme Park Featuring Mario And Harry Potter Opens In May—Here’s What We Know
- 13 Best Flower Delivery Services To Show Your Love From Miles Away
- What We Know About The Nicki Minaj-Megan Thee Stallion Feud—From ‘Hiss’ To ‘Big Foot’
- Taylor Swift At The Super Bowl: The Conspiracy Theory, Explained
- Crypto Is Suddenly Braced For A Huge China Earthquake After Bitcoin, Ethereum, XRP And Solana Price Surge